Global Investigation into Medical Devices Exposes Flaws in FDA, International Regulators
What medical device flaws mean for healthcare organizations.
The Implant Files raised concerns about how the FDA and other regulators assess medical devices.
In 2014, a Dutch journalist used a bag of mandarin oranges to fool European medical device regulators. Jet Schouten submitted the grocery store netting to three regulatory bodies, claiming it was a vaginal mesh. All three bodies approved the product.
That experience led to the Implant Files, a global investigation and database from the International Consortium of Investigative Journalists that looks at how medical devices are approved and recalled in 36 countries — and how a lack of reporting and transparency can lead to patient harm.
>> BRIDGE THE CLINICAL DIVIDE: Innovating Medical Devices for Patient Safety
In the United States, a decade of data from the Food & Drug Administration revealed more than 80,000 deaths and 1.7 million injuries potentially linked to medical devices, based on reports to from patients, doctors and medical device companies.
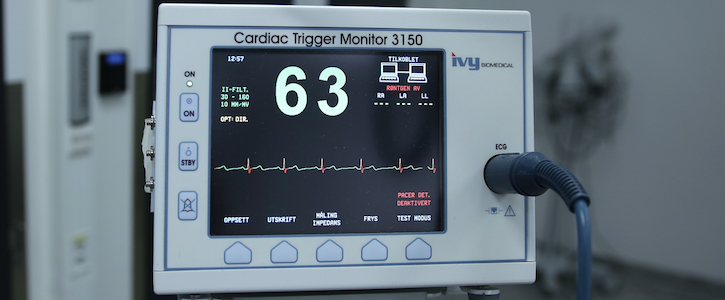
Healthcare providers are the vanguard in the medical device industry. And while the majority of approved devices — from breast implants to pacemakers — are improving lives, the investigation demonstrates that it is crucial for healthcare providers to be selective in vetting devices, in order to protect patient safety and their own investment.
At issue is both how medical devices get approved, and how problems are reported once they’re in use.
While the FDA has stricter guidelines than those in other countries, medical devices do not need to undergo clinical trials. The majority of devices — over 95 percent, according to the Associated Press — are fast-tracked to market under a process in which companies need only to prove that they are “substantially equivalent” to a product already on the market, even if that product is decades old, or has a history of problems. (The FDA is taking steps to overhaul the predicate process.) The agency has banned only two devices in more than four decades, according to the AP, and the average time for approval has decreased from more than 250 days two decades ago, to less than 100 today, according to the Implant Files.
In terms of tracking problems with devices, the FDA relies on reports from healthcare providers and device makers, who are supposed to file an adverse event reports when a device is suspected of malfunctioning or contributing to health problems. But the self-reporting can lead to flawed and incomplete data.
A primary example are insulin pumps, which are second only to metal hip replacements in the number of problems reported to the FDA, and yet many patients remain unaware of the potential risks. That’s because in many cases companies point to incorrect use as the source of the problem rather than their devices. Over the last decade, more than 100 lawsuits have been filed against Medtronic, which makes insulin pumps and pump parts, alleging pulp malfunctions, the investigation found. More thanr 150,000 reports have been submitted to the FDA involving Medtronic products since 2008. But in all those reports alleging injury or death, the company only documented a specific problem in 2 percent of cases, and in 80 percent they claimed that they could not determine the cause of the problem.
In November, the FDA put out a statement regarding its strategy for post-market safety of medical devices. According to the statement, the agency approves roughly 12 devices a day, after a careful determination “based on valid scientific evidence” that the devices are safe. The statement outlined ways for better post-market surveillance of medical devices, saying that better data is “one of the core pillars” of their safety plan.
The agency also ramped up its efforts to boost the cybersecurity of medical devices, which are increasingly interconnected to sensitive systems.
A final issue addressed by the investigation is the international implications of problems, which might go reported in one country and unnoticed in others. To that end, the authors of the Implant Files published a searchable database with records on medical recalls from all the countries involved in the investigation.
Get the best insights in healthcare analytics directly to your inbox.
Related
FDA Wants to Push Medical Device Makers to Innovate Beyond Old Predicates
Can Amazon Alexa Increase Patient Engagement?
FDA Bets on Real-World Evidence