HIMSS 2022: Health equity, transformation, Michael Phelps, Scott Pelley, and other highlights
The conference highlighted exciting opportunities for technology to dramatically improve healthcare, along with some formidable obstacles. Here are nine key takeaways from a memorable week.
The HIMSS Conference is history, but it generated conversations and ideas that should for some time.
The HIMSS Global Health Conference & Exhibition took place in Orlando last week, bringing together thousands of people and hundreds of sessions on healthcare technology and the transformation of medicine and healthcare.
Here are nine key takeaways from a memorable week.
Health equity
It’s not just a catchphrase or flavor of the month. Top healthcare leaders and federal officials repeatedly stressed that health equity is an extraordinarily high priority now, particularly in the wake of the COVID-19 pandemic.
Nine out of 10 healthcare executives said health equity is a core priority, according to a survey released by HIMSS and Accenture.
“We wouldn’t be having the same conversation 10 years ago,” said Ankoor Shah, management consulting principal director and health equity lead at Accenture.
In a video address at the conference, U.S. Health and Human Services Secretary Xavier Becerra talked about the federal government’s focus on health equity.
“We’re putting equity at the center of every decision we make,” Becerra said.
New penalties coming
The federal government is intent on seeing healthcare organizations share data more freely, partly toward that goal of health equity. And Becerra warned that there are going to be some new penalties coming for organizations that are blocking access to information.
Becerra talked about the complaints the health and human services department has received regarding organizations barring access to patient data. More than 75% of the complaints about information being blocked have involved healthcare providers, Becerra said.
“Closing this enforcement gap is an HHS priority,” Becerra said.
Becerra didn’t specify the penalties yet, but he said to expect some news on enforcement measures this year.
Telehealth isn’t going away
Virtually everyone agreed that the dramatic expansion of telehealth over the past two years is here to stay.
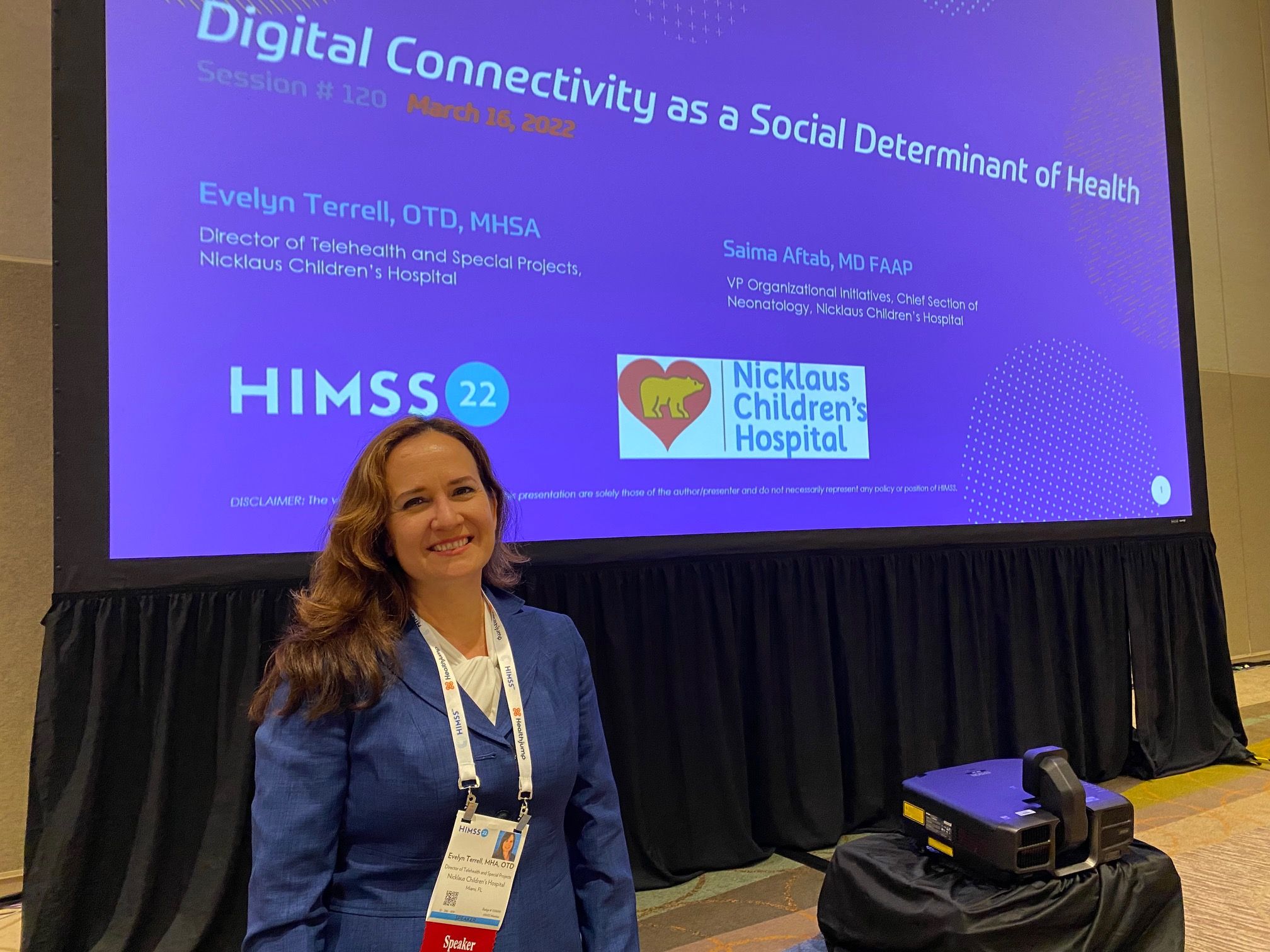
Evelyn Terrell, director of telehealth at Nicklaus Children's Hospital
However, there’s plenty of concern about making sure everyone has access to telehealth. Some studies have shown Black Americans and other members of minority groups have less access to video telehealth services.
Evelyn Terrell, the director of telehealth and special projects for the Nicklaus Children’s Hospital in Miami, Florida, outlined some thoughts on expanding access to telehealth at the HIMSS conference.
Part of those efforts including offering telehealth services in other languages and making sure older patients can use the technology easily.
Other experts at HIMSS talked about making sure telehealth is easy to use, both for patients and providers. They stressed the importance of helping physicians use the technology.
An ongoing concern: Will there be lasting telehealth reform from Washington? The government eased restrictions on telehealth in the pandemic, and the new federal budget includes a five-month extension of telehealth coverage after the public health emergency ends. But healthcare leaders want to see permanent access to telehealth services.
Going digital, but slowly
Yes, the digital transformation of healthcare is happening, but it’s not happening as quickly as it should be happening.
A panel discussion on the digital transformation of healthcare at the HIMSS 2022 Conference.

A panel at HIMSS offered perspectives from providers, patients, doctors, and payers. They all cited various obstacles and opportunities, but they all shared the same sentiment: it’s time to move more quickly.
Many patients are going to retail clinics, and those establishments are proving to be an appealing option for younger patients, said Lauren Goodman, HIMSS’ senior insight director and a marketing expert.
Healthcare providers have plenty of incentive to move to personalized care, she said.
“Those organizations will flourish,” she said. “Otherwise they might become obsolete.”
Bad managers are costing hospitals
There’s been plenty of discussion about the shortage of healthcare professionals, a common complaint across the industry.
Johnny Taylor, president and CEO of the Society for Human Resources Managers, talks at the HIMSS Conference Wednesday.

At a panel hosted by Scott Pelley of “60 Minutes,” experts said it’s time to face an uncomfortable truth.
Some of these workers are leaving because their bosses are driving them out.
Johnny Taylor, president and CEO of the Society for Human Resources Management, drew hearty applause for his observation that too many managers lack people skills.
“People don’t quit companies and hospitals and facilities,” Taylor said. “They quit their managers.”
Other seminars at HIMSS focused on giving doctors the tools and the time to learn new technology, and to incorporate their feedback in devising and implementing digital solutions.
Cybersecurity worries loom large
Healthcare executives have labeled cybersecurity as one of their top concerns, so it makes sense that a number of sessions at the HIMSS conference focused on the issue.
Ransomware has received plenty of attention, and healthcare organizations can expect more ransomware attacks in the near future.
Srinivas Loke, the senior director, product management at Ordr, a cybersecurity company, warned many breaches aren’t discovered for months and stressed the importance of bolstering defenses and developing good plans to respond when breaches occur.
Christian Dameff, an emergency physician and cybersecurity expert, said the risks to patient safety from cyber attacks merit much more attention. With more consolidation in the healthcare industry, if there’s a breach at one hospital in a healthcare system, he warned, “It’s not just one hospital going down, it’s five or six,” he said.
Michael Phelps discussed his mental health advocacy, and his personal struggles, at the HIMSS Conference Friday.

Michael Phelps talks about mental health
He’s the most decorated Olympic athlete of all time, but Michael Phelps has wrestled with depressions and thoughts of suicide.
He talked about his struggles candidly in the closing session of the conference. He also talked about his advocacy for mental health issues, including the importance of eliminating the stigma that keeps people from getting the help they need.
Phelps said he hoped to “change the mental health world.”
He also said he views his work on mental health as far more important this amazing feats in the swimming pool.
“To be able to have a chance to save a life is a million times better than winning a gold medal,” Phelps said. “I want to make an impact and I want to save lives.”
’60 Minutes’ would have been ideal
At the beginning of Wednesday morning’s keynote address, Scott Pelley joked that he’s used to having a full hour for “60 Minutes,” but he was limited to 45 minutes at HIMSS.
Pelley moderated the panel of experts in a discussion of the healthcare workforce. Given his preparation and perceptive questions, Pelley clearly could have moderated a discussion that lasted an hour, or two.
During the session, Pelley asked about the number of healthcare workers who have left the profession, citing numbers that were likely familiar to many in the audience. But then he asked a sharp question: How do we reignite the idea of the healthcare profession as a calling?
The question triggered a lively discussion about the importance of healthcare leaders showing empathy and support for healthcare workers. Tamara Sunbul, medical director of clinical informatics for Johns Hopkins Aramco Healthcare, emphasized the importance of manage of managers listening and engaging their employees.
“See what you can do to empower these healthcare professionals to do what they do best,” Sunbul said.
The panelists didn’t discount the importance of compensation. But they also said managers that listen to their employers’ concerns, and act on them, have a better chance of keeping their employees.
Pelley asked the right questions, and gave the panelists the space and time, to ensure a lively discussion.
Listen and act
Digital tools can enable healthcare providers to get a clearer picture of their health needs.
However, it’s not just enough to gather information. Baligh Yehia, an executive at Ascension, talked about his system’s efforts to identify the needs of their patients and then to get them help.
As Ascension began seeking information about unmet needs, some clinicians said they shouldn’t be asking about problems without offering to get them some help.
“When you think about designing programs, it’s not just a questionnaire,” he said. “It’s about, how do you put in place very specific interventions?”
Healthcare leaders: Prepare for a very different HIPAA security rule | Viewpoint
April 20th 2025The proposed changes to the HIPAA Security Rule are significant. Executives and boards need to prepare as the days of voluntary compliance end and a new era where leaders are held personally accountable emerges.
Telehealth faces a looming deadline in Washington | Healthy Bottom Line podcast
February 12th 2025Once again, the clock is ticking on waivers for telemedicine and hospital-at-home programs. Kyle Zebley of the American Telemedicine Association talks about the push on Congress and the White House.