The Top 4 Veterans' Health Stories of 2017
Several developments from 2017 promise to change, and hopefully improve, healthcare for veterans. Here are the top 4.
(Armistice Day in Kansas City, 1940. Photo courtesy Wikimedia Commons)
Veterans fall into a unique space in the healthcare system. There are more than 20 million military veterans who live in the United States, and the group has a far higher likelihood of suffering specific chronic and mental conditions than the general population. The Department of Veterans Affairs (VA) health system, however, is facing widespread staff shortages, complicating the country's ability to care for those patients.
Several developments from the past year promise to change, and hopefully improve, the unique healthcare situation that American veterans face. Here are the top 4 that Healthcare Analytics News covered in 2017.
A host of companies created or expanded relationships with the VA in 2017 to bring their services to veterans. In one of the most intriguing moves, the Department solidified its relationship with Personal Genome Diagnostics (PGDx), in November to advance precision medicine in the VA system.
“We are pleased that all eligible VA patients in the U.S. will now be able to obtain our advanced cancer genome testing and that our non-invasive, plasma-based cancer assays will be available to the many veterans who lack access to archival tissue samples, such as those in rural areas,” PGDx CEO Douglas Ward said.
3.
2017 saw the release and validation of several novel treatments for post-traumatic stress disorder (PTSD), including the use of “virtual humans” to interview veterans about their symptoms. A study out of the University of Southern California found that vets were more willing to open up to the computer-generated people than they were on completely anonymized surveys.
"These kinds of technologies could provide soldiers a safe way to get feedback about their risks for post-traumatic stress disorder," said Gale Lucas of the University of Southern California’s Institute for Creative Technologies. "By receiving anonymous feedback from a virtual human interviewer that they are at risk for PTSD, they could be encouraged to seek help without having their symptoms flagged on their military record."
2.
In November, the House of Representatives passed the
“This bill will ensure that our veterans receive timely health care no matter where they live,” one of the bill’s authors, Rep. Glenn Thompson (R-PA), said. The VETS Act received overwhelming support and was passed by verbal vote, signifying a small victory for veterans, telehealth, and bipartisanship alike.
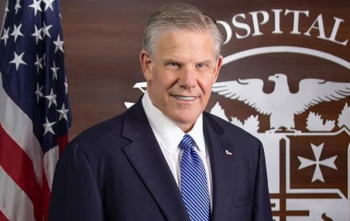
The biggest story involving veterans’ health this year was the VA’s decision to link with Cerner as its EHR provider. When VA Secretary David Shulkin began his term, he emphasized the importance of “getting VA out of the software business.” This summer’s contract announcement spells the end for VistA, the VA’s homemade, legacy EHR system. VistA is widely credited with being the first software of its type, but its development began decades ago and it was widely considered outdated.
The Cerner deal came, in part, because the Department of Defense (DoD) had chosen the provider to handle its patients’ EHRs in 2015. The hope is that having both departments on the same system will ease the transfer of medical records as service members transition from active duty into veteran status.
The move will not, however, come cheap. Trying to align its changeover with the DoD’s, the VA
The expense would require hundreds of millions of dollars to be repurposed from the VA medical care budget allotted for fiscal year 2018. Shulkin said that funding would have been used to purchase medical equipment that could be procured later, though critics in Congress pointed out that the VA’s 2018 budget already includes an unrelated $245 million cut in medical equipment spending.