Physician shortage could reach 86,000, AAMC projects
The Association of American Medical Colleges said the shortfall of doctors could make it harder for patients to get treatment.
Healthcare leaders warn that there’s already a shortage of physicians in America, and a new report suggests the problem could get worse in the coming years.
In a new
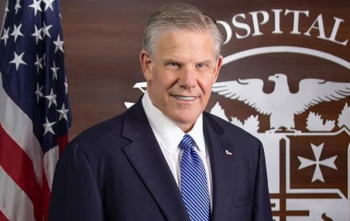
David J. Skorton, MD, the AAMC’s president and CEO, said the nation must invest to develop a new generation of doctors.
“We are looking at substantial shortages of doctors that will not meet our future health care demands,” Skorton said in a statement.
The AAMC report estimates the physician shortage as ranging between 13,500 and 86,000 by 2036. The AAMC estimates a shortage of between 20,200 and 40,400 primary care physicians, and a shortage of between 10,100 and 19,900 physicians in surgical specialties.
The AAMC’s projections are actually lower than
But the AAMC said that Congress must continue to invest in graduate medical education.
“The medical education community and policymakers are making real progress in our efforts to meet the projected health care needs of our communities, but we must not be complacent,” Skorton said. “We must continue to work with Congress to build on their recent bipartisan investments in Medicare-supported graduate medical education.”
With Americans growing older, the AAMC and other healthcare leaders say there’s going to be a need for more doctors. The number of Americans who are 65 or older is expected to grow by 34% by 2036. And older Americans typically have more healthcare needs, the AAMC notes.
America’s physician workforce is also graying and moving toward retirement age in the coming years. One in five doctors (20%) are 65 or older, and another 22% are between the ages of 55 and 64.
As seasoned doctors get ready to retire, the nation will need more doctors.
“Given the new findings, it is clear that both sustained and increased investments in training new physicians are critical to mitigating projected shortfalls of doctors needed to meet the health care needs of our country,” Skorton said in a statement. “Most importantly, if additional investments critical to increasing the supply of physicians fail to materialize, projected shortfalls of doctors will be larger than presented in this latest report.”
Hal Wolf, the president and CEO of HIMSS, has cited the shortage of physicians in talking about the need to accelerate the digital transformation of healthcare.
“It just simply doesn't work mathematically,” Wolf said at the HIMSS Global Health Conference & Exhibition last week. “Too many patients, too many needs, and frankly not enough clinicians.”
Medical schools have been enrolling more students in recent years. Since 2002, America’s medical school enrollment has risen by nearly 40%, according to AAMC data.
The AAMC has also pointed to the need to attract a more diverse group of students to meet the nation’s healthcare needs.
Healthcare leaders have also stressed