More than 1 million have lost Medicaid coverage, and hospitals are seeing the effects
States are determining some recipients are no longer eligible. Hospitals are providing more charity care, an indication that some have lost coverage.
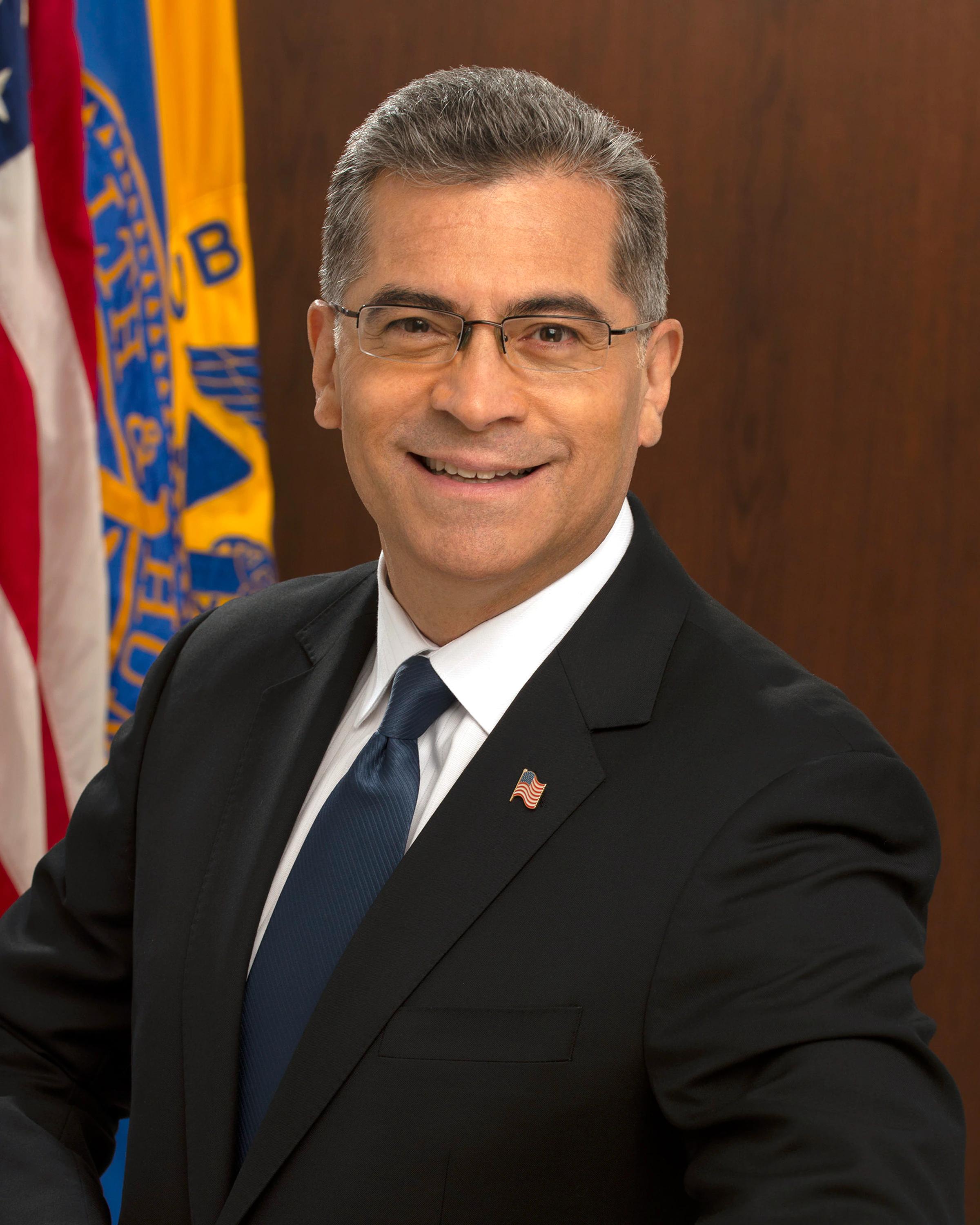
U.S. Health and Human Services Secretary Xavier Becerra is urging states to ensure that people who qualify for Medicaid get the assistance. More than 1 million Americans have lost Medicaid coverage in recent weeks. (Image: HHS)
As states once again have more latitude in determining eligibility for Medicaid, some Americans are losing coverage.
About 1.5 million Americans have lost Medicaid coverage in more than two dozen states, according to an analysis by The Associated Press.
Florida has dropped several hundred thousand people, far surpassing all other states, the AP reports. Arkansas has also dropped more than 140,000 people from coverage.
During the COVID-19 pandemic, state Medicaid rolls expanded significantly. States were told they needed to offer continuous Medicaid coverage in order to qualify for additional pandemic assistance. Under a federal spending package President Biden and Congress approved late last year, states were again given the ability to make their own determinations on Medicaid enrollment.
Nationwide, more than 93 million Americans were enrolled in Medicaid as of February 2023, up from 71 million in early 2020, according to the Centers for Medicare & Medicaid Services.
Arkansas Gov. Sarah Huckabee Sanders has said that the state is simply ensuring that only those who are eligible for Medicaid are getting that assistance. “Those who do not qualify for Medicaid are taking resources from those who need them,” she said on Twitter in May.
Florida officials say they make multiple attempts to reach recipients before moving to end coverage, and more than 150,000 people did not respond to those efforts, the AP reported.
U.S. Health & Human Services Secretary Xavier Becerra has asked states to be careful to avoid cutting Medicaid eligibility to recipients who need assistance. Becerra sent a letter to the nation’s governors last week urging them to be sure people don’t lose coverage due to administrative hassles and to make sure people know what they need to do to apply for benefits.
“Given the high number of people losing coverage due to administrative processes, I urge you to review your state’s currently elected flexibilities and consider going further to take up existing and new policy options that we have offered to protect eligible individuals and families from procedural termination,” Becerra wrote.
Some hospitals appear to be seeing the effects of people losing Medicaid coverage. Health systems have begun providing more charity care and seeing more bad debt, even as hospitals saw fewer patients in May, according to Kaufman Hall, the healthcare consulting firm.
“With states conducting their Medicaid eligibility redetermination, it’s predicted that hundreds of thousands of people will ultimately become uninsured,” Erik Swanson, senior vice president of data and analytics with Kaufman Hall, said in a statement. “The data indicate that we may already be seeing the effects of disenrollment materialize with patients less likely to seek out the care they need and a continued rise in bad debt and charity care.”
It’s difficult to project how many Americans will lose Medicaid coverage. KFF estimates that anywhere from 8 million to 24 million people could lose coverage. A KFF analysis also found that many are losing coverage because they didn’t fill out the paperwork.
Becerra outlined steps states can follow to ensure people who are eligible for Medicaid don’t lose coverage, including spreading out renewals over 12 months and renewing recipients on the basis of their eligibility for the Supplemental Nutrition Assistance Program or Temporary Assistance for Needy Families.
The health secretary has said he’s especially concerned that children could lose out on coverage if their parents no longer receive Medicaid, and Becerra points out that kids are most likely still eligible to receive coverage through Medicaid and the Children’s Health Insurance Program (CHIP).
In his letter to the governors, Becerra also said the federal government will act, including requesting that states pause procedural terminations if necessary.
"Individuals must be afforded the due process to which they are entitled in order for states to continue to receive enhanced federal funding," Becerra said.