7 Eye-Opening Virtual Care Stories from 2018
From virtual reality to mobile videoconferencing, 2018 was a big year for virtual care.
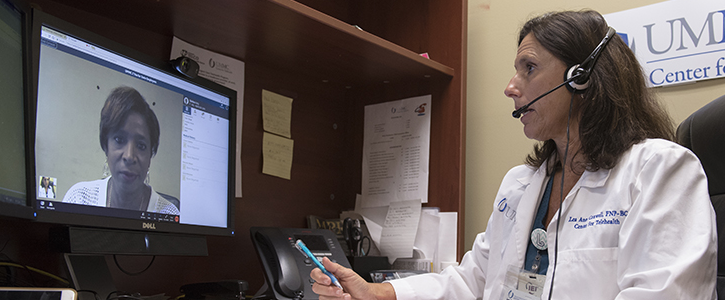
Virtual care is only going to continue to grow, whether patients like it or not. Physicians and hospitals have taken to integrating telemedicine services into their workflow, and even retail powerhouses like Walmart and Amazon are trying to get in on the action. And while one survey showed that most patients don’t engage in telehealth services, telemedicine has the potential to provide resources to people who experience trauma, hallucinations or social anxiety. Whether physicians are connecting with specialists via videoconferences, or radiologists are using telemedicine for patient interactions, it appears that virtual care flourished in 2018, and could be even more accessible and wide-ranging in 2019.
>> READ: Why CMS Is Betting on Telehealth Innovation
Picking only seven stories was no easy feat, as our site is full of articles about virtual care and telemedicine, but we compiled what we thought were our most informative pieces on the subject. So here they are, in descending order of course.
7. The First Real Measure of Telemedicine Use Is Here, and Small-Practice Docs Are Lagging
The American Medical Association conducted the first national study of 3,500 physicians to find the estimate of telemedicine use by physicians. While telemedicine use in hospitals flourished in practically every category, smaller practices did not use telemedicine often due to the financial burden of these tools.
6. Health Systems Must Beware of Retail Telemedicine
Mergers and acquisitions in healthcare have trended upwards in recent years. And the competition is on for health systems now that retail heavyweights like Walmart, CVS and Amazon are making the transition to healthcare by acquiring healthcare services and rapidly adopting telemedicine. The more companies that adopt these technologies the merrier, right? For patients, yes. They could have easier, cheaper access to doctors. Plus, retail outlets have physical locations and digital assets for patients to take advantage of. But let’s not forget that vertically integrated healthcare organizations already have established networks they can refer patients to for follow-up visits. Either way, we could be seeing a lot more telemedicine programs from both retail outlets and healthcare organizations in the near future.
5. How Telemedicine Helps Victims Heal After Tragedies
After tragedy struck Marjory Stoneman Douglas High School in Parkland, Florida in February, a telemedicine provider called MDLIVE was quick to offer their services. MDLIVE offered free, unlimited behavioral counseling services beginning the next day and through March to anybody affected by the shooting. Despite school officials declining the offer and opting for face-to-face treatment, it showed how far digitized behavioral health has come. Telemedicine is making it easier to recover from disasters and other traumatic events thanks to the growing acceptance of patients to seek treatment through mobile phones and computers.
4. When It Comes to Telemedicine, Patients Are Less Excited Than Doctors
More and more physicians are investing in telehealth. Conversely, a survey showed that less than 20 percent of patients use telehealth services. Why is this, and how should physicians incorporate these innovations into their workflow to educate patients about their benefits?
3. Digital Therapy Reduces Social Anxiety, Study Finds
A study at the University of British Columbia used a web-based program called Overcome Social Anxiety and found that the treatment group scored lower on both the Social Interaction Anxiety scale and the Fear of Negative Evaluation scale. A module-based cognitive behavioral therapy program, Overcome Social Anxiety allows people with the disorder who may generally worry about seeking treatment, the opportunity to get treatment while avoiding anxiety-inducing social situations.
2. VR is Helping Solve Schizophrenic Auditory Hallucinations
A new therapy, Audio Visual Assisted Therapy Aid for Refractory auditory hallucinations (AVATAR) is undergoing trials to aid patients affected by auditory hallucinations due to schizophrenia. Patients in AVATAR therapy build customizable visual representations of the voice in their heads. The results of a study showed a decrease in the patients’ Psychotic Symptom Rating Scale scores, but more research is required to see if AVATAR therapy could be instituted widely across clinics.
1. Video Counseling Can “Upskill” PCPs, Bringing Specialty Knowledge to Rural Patients
Primary care providers who participated in a program called SCAN-ECHO were more likely to follow the guidelines for proper treatment of liver disease. The program works to “upskill” physicians by connecting them — via video — to specialists to inform how to care for patients with unique needs. Programs like this provide better opportunities for patients, especially in rural areas, to receive proper care.
Get the best insights in healthcare analytics directly to your inbox.
Related Coverage
Using a Rising Telehealth Tide to Lift All Primary Care Physicians
Digital Health Investors Want Innovation, Even if Inspiration Comes from Fortnite
How Regence Determined Telehealth Was Saving $100 Per Appointment
Podcast: Adoption of Healthcare Tech in the Age of COVID-19 with Dr Kaveh Safavi
June 22nd 2021Kaveh Safavi, MD, JD, global health lead of Accenture Health, discusses how the pandemic influenced the speed at which healthcare organizations adopted new technologies and how this adoption is impacting patient care.